Strabismus is routinely encountered by ophthalmologists world over. It is known to occur in about 5 percent of the population. Strabismus surgery is a well described and ubiquitously performed surgery , albeit with unpredictable results.
Indications for strabismus surgery in children include ensuring alignment of eyes to prevent maldevelopment of sensory apparatus which can cause anomalous retinal correspondence , suppression and amblyopia. Another extremely common indication for squint surgery across all age groups is cosmetic deformity due to the deviating eyes. (Fig 1)
Studies that describe the psychological impact of crossed eyes reiterate that , in general , patients with squint are perceived as being less capable and less intelligent. Hence presence of strabismus can adversely affect a person’s quality of life , not just in terms of sensory maldevelopment but also the psychosocial aspects leading to a negative self image and low self esteem. This can further have an adverse impact on relationships , job prospects and educational opportunities. These facts have been substantiated by measurement of HR QOL (Health Related Quality of Life) in squint patients. HRQOL has been documented to improve significantly after squint surgery
Considering the ramifications of this disease , it is of utmost importance to ensure cure and successful outcome in patients who undergo surgical correction . The correction should be planned in such a way that we are certain of predictability, accuracy and reproducibility in the postoperative results.
Briefly, the major factors on which surgical outcome depends , can be classified as
- Surgeon related factors– Expertise and experience of the surgeon , meticulousness and attention to detail while performing the surgery, surgeon preference of a particular surgical technique , surgeon’s intuition and surgical sixth sense , to name a few .
- Patient related factors are largely – Age of the patient , Refractive error , Etiology and magnitude of squint , Anatomical variations , delays in seeking treatment and history of any previous squint surgery
To navigate successfully through the treatment process , outlined here , in this article ,is an indicative and experiential step by step guide for moving towards perfect outcomes-
- Importance of an all inclusive pre operative evaluation including complete motor and sensory evaluation cannot be over emphasized .
Pre operative angle of deviation is proven to be the strongest factor for predictability and success of squint surgery. It is measured with prism bars using Prism Bar Cover Test (PBCT) with documentation of two reproducible measurements on 2 different occasions .
Greater the pre operative deviation , better is the surgical outcome.
Studies have also shown that pre operative deviations of less than 30 PD tend to have a better surgical outcome.
Measurement outcome of PBCT can be further refined by
- PBCT after prolonged mono ocular occlusion
- PBCT at far distance
- Consideration for AC/A ratio , as per the clinical situation
Causes for erroneous PBCT measurements need to be borne in mind , as taking care of the following factors can lead to perfect outcomes-
- Amblyopia– Modified Krimsky test / PBRT is carried out for measuring deviation in amblyopes. Modifed Krimsky’s test is inherently less reliable than PBCT due to possibility of errors of parallax. Errors of parallax may be reduced by positioning examiner’s own eye directly or behind the handheld light. Modified Krimsky test may also give errors because of individual variability in angle kappa.
- Large deviations– Large deviations need higher prism powers for measurement. (Fig 2)Stronger the prism applied, greater are the chances of error .
Large deviations may also need splitting of prisms between two eyes or stacking of prisms in front of one eye. Generally , stacking of horizontal prisms is not recommended as prisms do not add up linearly and can really escalate probability of error. Splitting of prisms between the two eyes may also give error , though the magnitude is much lesser compared to stacking. Splitting of prisms can be practiced in large angle comitant strabismus .
Delineating the largest angle is of utmost importance for perfect cosmetic outcome. It prepares the surgeon for carrying out greater amount of surgery on the extra ocular muscles . This needs even greater care as larger surgery means more violation of muscle pulleys and possibility of orbital fat resection
- Combined vertical and horizontal deviation can also lead to variable PBCT findings. (Fig 3)This can be overcome by meticulous PBCT using stacking of horizontal and vertical prisms.
- High refractive error , and PBCT over thick glasses can also reduce the accuracy of the measurement. This occurs because of the prismatic effect induced by high refractive error of 5D or above. It should be remembered that plus glasses always measure less than actual deviation [both in eso & exo). Minus glasses always measure more than actual deviation [both in eso and exo].
- Proper refractive correction . Cycloplegic refraction before planning surgery, helps to identify those having significant refractive error . Glasses should be prescribed and worn regularly for the period of refractive adaptation , which may take upto 18 weeks , following which the magnitude of deviation should be ascertained by PBCT.
Certain types of squint get completely corrected with glasses such as accommodative esotropia (Fig 4) ; or get reduced substantially with glasses such as partially accommodative esotropia.
For patients having significant squint after glass correction , PBCT measurements with glasses are the target angle for surgical correction.
For myopic patients with strabismus , following additional points need to be borne in mind-
- As minus lenses increase the amount of measured deviation , it can lead to surgical overcorrection. Hence it is recommended to increase the measured deviation by 2.5%
- Planned undercorrection can be carried out , as per refractive error of the patient , based on Hansen’s data
- Measurement with contact lenses instead of glasses , to obviate the prismatic effect
- Careful surgery to avoid inadvertent scleral perforation due to thin myopic sclera
- Focus on the third dimension – Testing for three dimensional vision before surgery , can help to predict the outcome of surgery. Impaired binocular vision implies worse long term outcomes. Early detection of loss of stereopsis can be used to ensure timely intervention especially in intermittent deviations .
- Active management of lazy eye– – Pro active management of amblyopia should precede surgery. Traditional occlusion therapy can be combined with adjuncts such as oral citicoline for improved results. If compliance to routine occlusion therapy with patches is low , LCD glasses can be used for carrying out occlusion . Dichoptic training can help to achieve higher level of plasticity than occlusion alone.
- Binocular vision therapy pre operatively has been known to culminate into better post operative outcomes especially in terms of long term maintenance of orthotropia.
- Age at surgical intervention – Surgery done at a younger age leads to more response because of the small size of the eye. Age is of significance for infantile deviations also as it is recommended to operate on them by one year of age(Fig 5)
- Role of imaging – Imaging modalities such as CT scan , MRI , UBM , Swept Source AS- OCT have been used for understanding etiology and for planning surgery. For instance, high resolution MRI helps to define muscle pulleys . Heterotopic pulleys account for incomitant squint and pattern strabismus. Swept source AS- OCT / wide field UBM are used for detection of muscle insertion in previous operated /fresh cases. Dose response curve of previously operated EOMs differs from unoperated muscles. Imaging is especially required in case of non availability of previous records or if the re surgery is carried out by another Also patient information and history regarding type of strabismus and surgical history may be inaccurate. Additionally, stretched scars and muscle creep can change the insertion over years in previously operated cases
- Per-operative pearls– Hallmarks of a good squint surgery include meticulous dissection , reproducible technique , use of a microscope or loupe , good anesthesia – topical or sub tenon infiltration or general anaesthesia. Surgical trauma should be reduced to minimum as the subsequent surgical edema can cause refractive change by changing axial length and anterior chamber depth
- Adjustable sutures help to alter and adjust the surgical dose even post operatively in the form of a relatively simple and quick procedure which can be done under topical anaesthesia . It helps to improve short and long term outcomes by overcoming any unplanned under correction or over correction
- Botulinum toxin may be utilized in under or over corrections or as adjunct to surgery in large horizontal deviation , though reliance on botulinum toxin for enhancing squint outcomes is still not very widely practiced practically
- Minimally invasive squint surgery (MISS) -MISS has been shown to produce better outcome and earlier rehabilitation. Key hole incisions are the cornerstone of MISS. Advantages of MISS include reduced risk of post operative corneal complications , minimal post operative discomfort and better preserved muscle function. Also there are lesser chances of conjunctival congestion , chemosis , corneal dellen , tenon s prolapse because of minimal tissue disruption and minimal collateral damage. There are minimal chances of anterior segment ischaemia due to preserved perilimbal vasculature. MISS can be used to perform all types of surgeries .
- Type of surgery– Unilateral recess-resect may have better outcome than bilateral lateral rectus surgery especially in deviations upto 60 PD. Though it depends widely on surgeon’s preference and experience.
- Topical Brimonidine has been advocated quite recently intra operatively and post operatively, for the purpose of reducing conjunctival injection. Even with perfect ocular alignment , post operative conjunctival injection can be a significant source of anxiety and disappointment and a cosmetic issue. Advantages of topical brimonidine include lesser systemic adverse effects , can be safely used in children more than 2 years of age and may help to counter steroid induced increase in IOP
- Fibrin glue for conjunctival closure gives the advantage of lesser operating time / GA time , lesser inflammation which culminates in lesser conjunctival congestion , leading to better patient comfort and cosmesis
- Binocular vision therapy after strabismus surgery – Even after perfect post op ocular alignment , there are some chances of recurrence of misalignment. To reduce recurrence , binocular vision therapy is utilized for improving sensory and motor visual skills. It can be advocated as active office based therapy or home therapy or a combination of both. It encompasses anti suppression exercises along with fusional and accommodative exercises.
Perceptual learning and binocular integrative exercises result in improved binocular coordination and stereopsis

Fig 1. Cosmetic deformity due to squint

Fig 2. Large deviations

Fig 3. Combined horizontal and vertical deviation
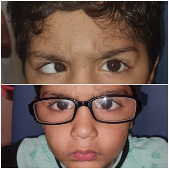
Fig 4. Accommodative esotropia

Fig 5. Timely intervention in infantile esotropia
REFERENCES
- Kumari N, Amitava AK, Ashraf M, Grover S, Khan A, Sonwani P.Prognostic preoperative factors for successful outcome of surgery in horizontal strabismus. Oman J Ophthalmol 2017;10:76–80.
- Magli A, Rombetto L, Matarazzo F, Carelli R. Infantile esotropia risk factors associated with reoperation. Clin Ophthalmol 2016;10:2079–83.
- Magli A, Carelli R, Matarazzo F, Bruzzese D. Essential infantile esotropia: postoperative motor outcomes and inferential analysis Of strabismus surgery. BMC Ophthalmol 2014;14–35.
- Ehrenberg M, Nihalani BR, Melvin P, Cain CE, Hunter DG, Dagi LR. Goal-determined metrics to assess outcomes of esotropia surgery. JAAPOS 2014;211–216.
- Astudillo P, Cotesta M, Scholfield J, Kraft S, Mireskandari K. The effect of achieving immediate target angle on success of strabismus surgery in children. Am J Ophthalmol 2015;160:913–8.
- Gogate PM, Rishikeshi N, Taras S, Aghor M, Deshpande MD. Clinical audit of horizontal strabismus surgery in children in aharashtra, India. Strabismus 2010;18:13–7.
- Louwagie CR, Diehl NN, Greenberg AE, Mohney BG. Long-term follow-up of congenital esotropia in a population-based cohort. JAAPOS 2009;13:8–12.
- Dickmann A, Aliberti S, Rebecchi MT, et al. Improved sensory status and quality of lifemeasures in adult patients after strabismus surgery. J AAPOS 2013; 17: 25–28.
- Andalib D, Nabie R and Poormohammad B. Factors affecting improvement of stereopsisfollowing successful surgical correction of childhood strabismus in adults. Strabismus 2015;23: 80–84.
- Kassem RR and Elhilali HM. Factors affecting sensory functions after successful postoperative ocular alignment of acquired esotropia. J AAPOS 2006; 10: 112–116.
Author Details
Dr Bhawna P Khurana
MS, DNB, FICO , FRCS(Glasgow)
Paediatric Ophthalmologist and Oculoplastics Specialist
Khurana Eye Centre
Email- drbhawnakhurana@gmail.com
