For the treatment of corneal endothelial disease there occurred a major shift from full thickness penetrating keratoplasty (PK) to component keratoplasty in last two decades. PK was used successfully for over a century for the treatment of endothelial disease but it requires months of follow up before eye achieves visual stability. Astigmatic error changes every time a suture has been removed and lower globe stability at the host graft interface maintains a clear risk of dehiscence even with trivial trauma years after the surgery. On the other hand with endothelial keratoplasty; only a portion of recipient cornea has been removed, comparatively smaller size graft has been transplanted thus a lesser foreign antigen exposure occurred, few or no suture has been placed and thus lesser astigmatism, lesser vascular ingrowth and chance of graft rejection, improved globe stability and faster visual recovery takes place.
Modern endothelial keratoplasty has evolved through Posterior Lamellar Keratoplasty (PLK)/ Deep Lamellar endothelial keratoplasty (DLEK) to Descemet’s stripping endothelial keratoplasty (DSEK)/ Descemet stripping automated endothelial keratoplasty(DSAEK) and then finally to Descemet’s membrane endothelial keratoplasty (DMEK).
So talking about the endothelial keratoplasty, DMEK is the current gold standard procedure and is rapidly being adopted because:
- DMEK presents significant visual improvement over DSEK; 95% of eye achieve >20/40 vision as compared to 43% in DSEK and 50% eye achieve >20/25 vision as compared to only 6% in DSEK, so if you look at the mean best corrected visual acuity (BCVA) result of these two DMEK is the winner.
- DMEK eliminates the need of automated microkeratome; thus increase in its ease of adaptation especially in the developing world.
- Graft does not have corneal stroma; no myopic shift as in case of DSEK/DSAEK.
- Faster visual rehabilitation and lesser risk of graft rejection.
- No induction of visual distortion and higher order aberration.
“BUT WHEN DMEK IS NOT A RIGHT OPTION”
- Poor visibility as after severe scarring / failed Penetrating Keratoplasty (PK).
- Aphakic bullous keratopathy.
- Large Peripheral iridotomy /sectoral iris defect.
- Anterior chamber intraocular lens (ACIOL).
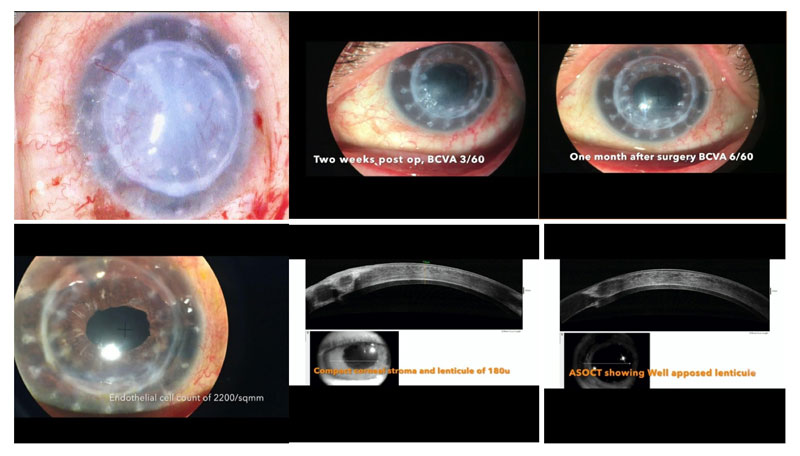
CASE 1:
A 60 year old lady with history of uncontrolled diabetes mellitus and hypertension presented with chief complaint of diminution of vision. The right eye was pseudophakic with mild non proliferative diabetic retinopathy. The left eye has failed Penetrating Keratoplasty, done for the scarring after viral keratitis three years back. Corneal thickness was found to be increased (1600um) with failed graft, severe superficial and deep vascularisation reaching up to the central cornea region. There was Cystoid macular oedema in the left eye. Manual DSEK followed by treatment of cystoid macular oedema was planned with explained high risk of graft failure due to uncontrolled DM and high risk of HSV keratitis as per previous history. Best corrected visual acuity (BCVA) of 3/60 noted after postoperative period of 2 weeks. The graft lenticule was found well opposed on AS-OCT. CME is now addressed and strict metabolic control for diabetes mellitus was advised. BCVA improved to 6/60 after postoperative period of one month, and some regression of superficial and deep vascularisation noted. At three month follow up cornea became completely avascular with BCVA 6/36 further improving to 6/18 after three years.
CASE 2:
Patient presented with the chief complaints of diminution of vision and foreign body sensation in LE. There was a history of cataract surgery with IOL implantation 15 years back. Pseudophakic bullous keratopathy developed later on, for which IOL explantation was done 3 years back elsewhere. Best corrected visual acuity (BCVA) of patient at presentation was 2ft. finger counting. Aphakic bullous keratopathy was found with severely oedematous cornea and hypertrophic corneal epithelium. A large superior sectoral iridectomy was also seen. Scleral fixated IOL with modified Yamane technique with DSEK was done. Postoperative one month visual outcome was 6/36 which improved to 6/24 after 2 months.

CASE 3:
Thirty eight year old myopic gentleman presented with chief complaints of diminution of vision with pain and redness. Uncorrected visual acuity (UCVA) was 1/60; best corrected visual acuity (BCVA) was 6/60. Intra ocular pressure was raised. There was a history of post traumatic dislocated Intraocular lens explantation with pupilloplasty with Scleral fixated intraocular lens implantation with Descemet Membrane Endothelial Keratoplasty (DMEK) done elsewhere, three months back. History of rebubbling postsurgery was also present. Severe corneal oedema with displaced graft obscuring half of the angle resulting into the raised intraocular pressure noted and scleral fixated intra ocular lens (SFIOL) seen. Patient was planned for removal of dislocated graft with manual Descemet Stripping Endothelial Keratoplasty (DSEK). After one month postoperatively best corrected visual acuity noted was 6/9 with clear graft and IOP in normal range.

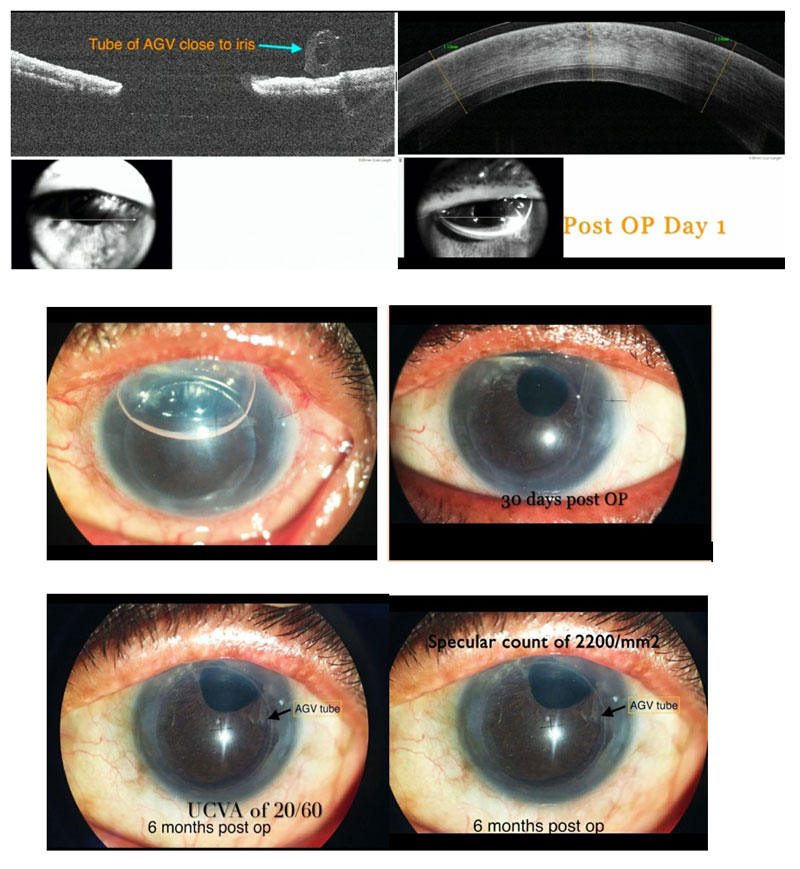
CASE 4:
An 80 year old gentleman presented with the chief complaints of severely diminished vision in the only Seeing Eye. He was a known case of primary open angle glaucoma in both eyes and was on antiglaucoma medications. His right eye had glaucomatous optic atrophy. He was pseudophakic in left eye with uncontrolled IOP with maximum tolerated antiglaucoma medications. BCVA in left eye was 20/600. His endothelial cell density was 575/mm2. He underwent AGV first to control IOP. Six months after the IOP was under control limited anterior vitrectomy with manual non DSEK was done using Busin Glide. Graft was well opposed on post op day one. Six month post op UCVA was 20/60 and BCVA was 20/30. Endothelial cell density was 2200/mm2.
CONCLUSION:
DMEK is the gold standard for endothelial dysfunction but DSEK/DSAEK comes in handy in difficult situation.
By,
Dr Praveen Dhanapal,
Cataract, Cornea & Refractive Surgeon,
Ratan Jyoti Netralaya Institute of Ophthalmology and Research Centre,
Gwalior, Madhya Pradesh
