Authors
Deepanshu Agrawal (DO, DNB, FVRS),1 Dhaivat Shah (MS, DNB, FMRF),2 Ashima Monga (DNB)3
Affiliations
Consultant, Vitreoretina and Uvea Services, Choithram Netralaya, Indore, Madhya Pradesh, India
Consultant, Vitreoretina and Uvea Services, Head Academics and Research, Joint Medical Director, Choithram Netralaya, Indore, Madhya Pradesh, India
Fellow, Medical Retina, Choithram Netralaya, Indore, Madhya Pradesh, India
Corresponding author:
Dr Deepanshu Agrawal
Consultant, Vitreoretina and Uvea Services
Choithram Netralaya, Indore, Madhya Pradesh, India
Email ID: deep.ansh2007@gmail.com
Phone No.: +91-9008479737
Bacillary Layer Detachment: Unraveling the Mechanisms and Management
By definition bacillary layer detachment (BLD) is separation between myoid and ellipsoid zone of the inner segment of the photoreceptors which occurs following trauma or subsequent to inflammatory insult to the outer retina.[1] It has been described in cases of VKH disease, toxoplasma retinochoroiditis, central serous chorioretinopathy, acute posterior multifocal placoid pigment epitheliopathy. In the current case report, we highlight the characteristic clinical presentation, management and outcome of this OCT based entity in a case of choroidal tubercular granuloma.
A 30-year-old-male, presented with complaints of left eye sudden painless diminution of vision for 2 days. There was no other significant systemic, personal or similar past history. On evaluation his best corrected visual acuity in the right (OD) and left eye (OS) was 20/20 and 20/320, respectively. Slit lamp examination revealed clinically unremarkable anterior segment, bilaterally, with no signs of inflammation. On dilated posterior segment evaluation clear media was noted, with no retrolental cells or vitritis. OD fundus evaluation was within normal limits. However, in OS, posterior pole had a sub-retinal lesion (~1DD in size) present inferior to the fovea, above the inferior arcade along with presence of sub-retinal fluid involving fovea. There were few healed choroiditis patches, temporal to the current area of activity [Figure 1a]. Patient had no past history of any previous systemic or ocular treatment. The healed lesions had most likely resolved spontaneously.
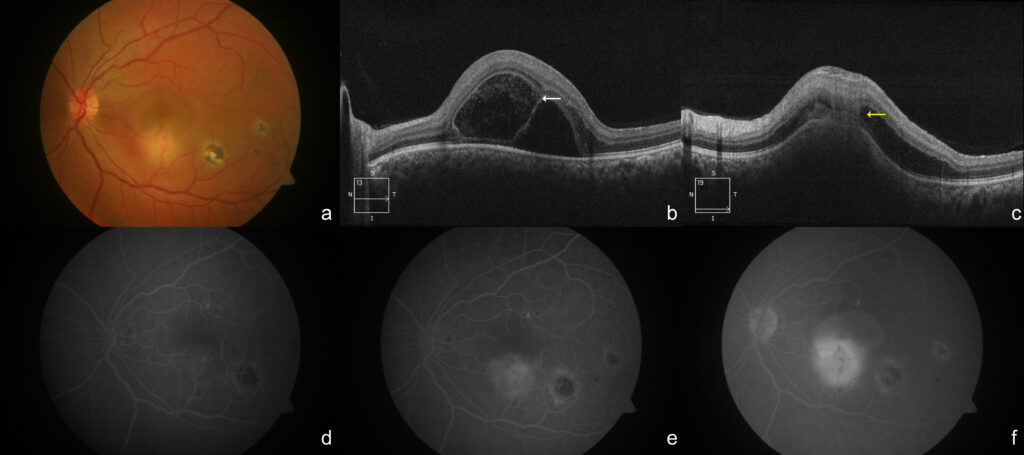
Patient was subjected to optical coherence tomography (OCT) and fundus fluorescein angiography (FFA) of the left eye. OCT revealed presence of large area of BLD with concurrent presence of neurosensory detachment at the level of fovea and presence of choroidal elevation along with contact sign, noted in the center of the lesion [Figure 1b,c]. FFA elicited a well-defined area in the early phase which turned hyperfluorescent in the later stage [Figure 1d-f]. With provisional diagnosis of Choroidal Granuloma, patient was advised uveitis workup (Complete blood count, HIV, TPHA, Mantoux test, interferon gamma release assay, Serum ACE, HRCT – Chest). Systemic investigations revealed a positive Mantoux test (Induration: 20mm*15mm) and positive interferon gamma release assay (IGRA). HRCT – chest was within normal limits.
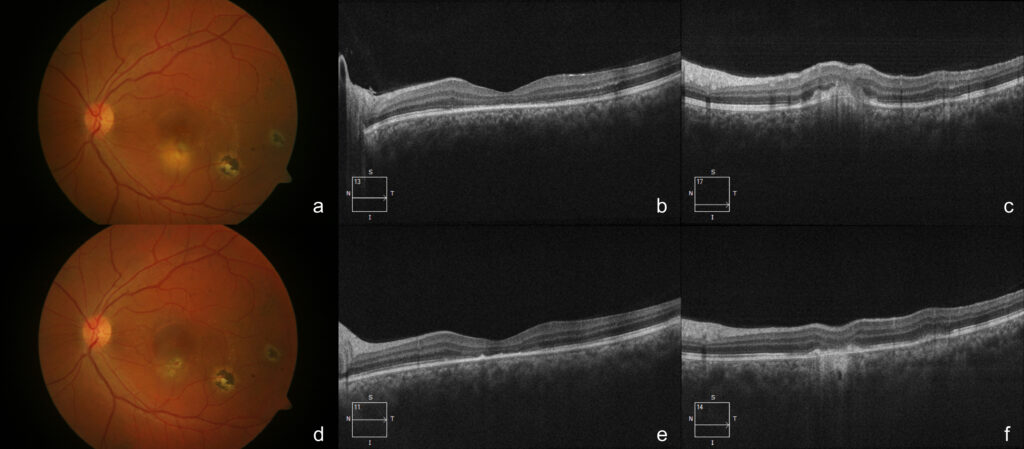
Treatment: Pulmonologist opinion was sought and patient was started on dual therapy of anti-tubercular therapy (4 drug regime) along with oral steroids (1mg/kg; body weight=72kg). On 1 week follow-up we noted a very quick response to the dual therapy as there was complete resolution of sub-retinal fluid along with settlement of BLD. [Figure 2a-c] Sub-retinal lesion had completely resolved with a scar on 1 month follow-up. [Figure 2d-f] Post-resolution BCVA improved to 20/32 (OS), with loss of outer retinal layers at fovea (on OCT). Systemic steroid was tapered on weekly basis (10mg/week) and subsequently stopped. Anti-tubercular therapy was continued for a period of 6 months (2 months HRZE + 4 months HR).
Bacillary layer detachment (BLD) terminology was coined by Mehta et al.[1] Anatomically, photoreceptor inner segment comprises of two parts, proximal myoid layer and distal ellipsoid zone. The ability to undergo retinomotor contraction led to the term myoid zone. It mainly comprises of protein producing organelles like Golgi apparatus, ribosome, and endoplasmic reticulum. However, the ellipsoid zone comprises mainly of mitochondria. By definition BLD is separation between myoid and ellipsoid zone of the inner segment of the photoreceptors which occurs following trauma or subsequent to inflammatory insult to the outer retina.[2] Due to separation of these two layers, fluid accumulation occurs in intra-photoreceptor space and leads to detachment.
Mycobacterium Tuberculosis is the causative agent for the tubercular infection. Tuberculosis mainly has systemic predilection. However, it can rarely involve only ocular structures and more commonly it presents as posterior uveitis, affecting the choroid. TB Granuloma usually presents as multifocal lesions, less commonly they can be seen as solitary, defined lesion at the posterior pole.[3] These lesions on OCT are seen as choroidal elevation along with presence of subretinal fluid. Another peculiar feature of TB Granuloma is presence of attachment between neurosensory layers along with retinal pigment epithelium with inflammatory infiltrates in between, over the area of choroidal Granuloma, popularly known as “Contact Sign” (noted on OCT).[4,5] Once the clinical findings and systemic investigations like Mantoux test and interferon gamma release assay (high specificity) test, correlates and helps in confirming the diagnosis, then patient can be started on concurrent treatment regime of the anti-tubercular therapy and systemic corticosteroid, which results in faster settlement of BLD as well as quick resolution of choroidal granuloma. In our case, time to near complete resolution was 1 week and it completely subsided at 1 month follow up, with a flat scar over the involved area.
Bacillary layer detachment is a recent OCT based entity. As seen in the current case and also in the previously reported cases of BLD, splitting of inner retinal layers occur at the level of ellipsoid zone. In the year 1941,[6] neuroanatomist Polyak had described this as bacillary layer. Previously these collections of fluid were being described as huge outer retinal cystic space, outer retinal fluid, sub retinal fluid with fibrin, etc. The terminology of BLD was first proposed by Mehta et al. [1] which was coined to denote these similar presentations. Mehta et al. had reported splitting of the bacillary layer; case described by them had similar findings to that of our case. known to occur in ocular conditions like Vogt-Koyanagi-Harada disease, Exudative age-related macular detachment, acute posterior multifocal placoid pigment epitheliopathy, unilateral acute idiopathic maculopathy, pre-eclampsia, retinochoroiditis secondary to toxoplasmosis, and ocular trauma.[7,8] It has seldom been reported in a case of choroidal tubercular granuloma.[9] Therefore, this case uniquely highlights key points in clinical assessment, diagnosis and management of the case.
References:
- Mehta N, Chong J, Tsui E, Duncan JL, Curcio CA, Freund KB, et al. Presumed Foveal Bacillary Layer Detachment in a Patient with Toxoplasmosis Chorioretinitis and Pachychoroid Disease. Retin Cases Brief Rep.2018;15:391-8.
- Ramtohul P, Engelbert M, Malclès A,Gigon E, Miserocchi E, Modorati G, et al. Bacillary layer detachment: multimodal imaging and histologic evidence of a novel optical coherence tomography terminology: literature review and proposed theory. Retina. 2021;41:2193-207.
- Bodaghi B, LeHoang P. Ocular Tuberculosis. Curr Opin Ophthalmol. 2000;11:443-8.
- Yeh S, Sen HN, Colyer M, Zapor M, Wroblewski K. Update on ocular tuberculosis. Curr Opin Ophthalmol. 2012;23:551-6.
- Salman A, Parmar P, Rajamohan M, Vanila CG, Thomas PA, Jesudasan CAN. Optical coherence tomography in choroidal tuberculosis. Am J Ophthalmol. 2006;142:170-2.
- Polyak SL. The Retina: The Anatomy and the Histology of the Retina in Man, Ape, and Monkey, Including the Consideration of Visual Functions, the History of Physiological Optics, and the Histological Laboratory Technique. Chicago: University of Chicago Press; 1941.
- Cicinelli MV, Giuffré C, Marchese A, Jampol LM, Introini U, Miserocchi E, et al. The bacillary detachment in posterior segment ocular diseases. Ophthalmol Retina 2020;4:454‑6.
- Kohli M, Bhatia P, Shenoy P, Sen A, Gupta A. Bacillary Layer Detachment in Hyperacute stage of Acute Posterior Multifocal Placoid Pigment Epitheliopathy: A Case Series. Ocul Immunol and Inflamm. 2022;30:703-6.
- Markan A, Aggarwal K, Gupta V, Agarwal A. Bacillary layer detachment in tubercular choroidal granuloma: A new optical coherence tomography finding. Indian J Ophthalmol 2020;68:1944-6.
