During the aging process, the face loses fat and volume; the skin loses collagen and elasticity. Young faces have full cheeks and curves but the aging face becomes framed by bony contours wrapped with thin skin, lending a deflated and fallen appearance. The use of botulinum toxin can reduce the appearance of wrinkles but it doesn’t correct the volume loss. The placement of injectable fillers in the treatment of lines, wrinkles, and areas of volume depletion can achieve excellent aesthetic results with limited or no downtime and without the potential morbidity of surgery.
Dermal fillers are injectable materials consisting hyaluronic acid, Calcium hydroxylapatite, Poly – L – lactic acid among others. These materials are injected to add volume to the face and can help regain the full, youthful look. They are used to add volume to the cheek, the temple, tear tough deformity and even in the treatment of wrinkles.
Figure 1: Here, a 35-year-old female underwent a dermal filler injection (Juvederm) in the tear trough area. Filling in the right area obliterated the valley or depression to create a smooth lid cheek transition correcting her ‘tired’ looking eyes, dark circles and lower eyelid wrinkles.

However, not all uses of dermal fillers are cosmetic. Over time, clinicians have been able to harness the advantages of filler injections – the ease of use, temporary effect, reversibility and less complications to treat non-cosmetic functional issues as well. Here we will be highlighting two such conditions where dermal filler offer a viable, effective, minimally-invasive option to surgery: epiblepheron and lagophthalmos.
1. Epiblepheron:
Epiblepharon is a common eyelid disorder in children characterized by an abnormal eyelid fold with resultant in-turning of lashes and irritation of ocular surface. This can cause epiphora and corneal epithelial defects. Also, conjunctival epithelial metaplasia due to in-turned lashes and induced astigmatism due to squeezing have been reported in these patients. The hypothesized causes for epiblepheron include failure of eyelid retractors to gain access to the eyelid skin and hypertrophy of orbicularis muscle.
Figure 2: Epiblepheron in a 6 month old child – Note the extra fold of skin seen on the lower lid with the lashes turned inwards rubbing on the cornea

Traditionally, epiblepharon is believed to correct itself with advancing age, and surgical correction is required only for severe cases. Since it is a self-correcting condition, a permanent surgery may not be always required. In mild cases, conservative management in the form of topical lubricants can be advised. Severe cases with keratopathy may require surgical correction, and there are many different surgical techniques that have been described. However, there is no standardized uniform surgical correction, or normograms that can serve as a guide to how much of skin-muscle needs to be excised. Also, the condition has not been studied in detail enough for any one surgical technique to have clear objective pre-operative parameters to decide which surgical technique is most beneficial. Therefore in these cases, a temporary filler injection could be used to treat the epiblepheron.
As Naik et al. have demonstrated, a filler injection of hyaluronic acid gel obliterates the valley above the skin fold, thereby providing a splinting effect, which prevents the abnormal skin fold to override and push the lashes inwards. When injected in the right area, the filler in the in the suborbicularis plane fills up the valley between the eyelid margin and the skin fold. Usually with 0.2-0.3 ml, the skin fold valley gets completely flattened and immediate eversion of the eyelid margin with resultant out-turning of lashes can be appreciated.
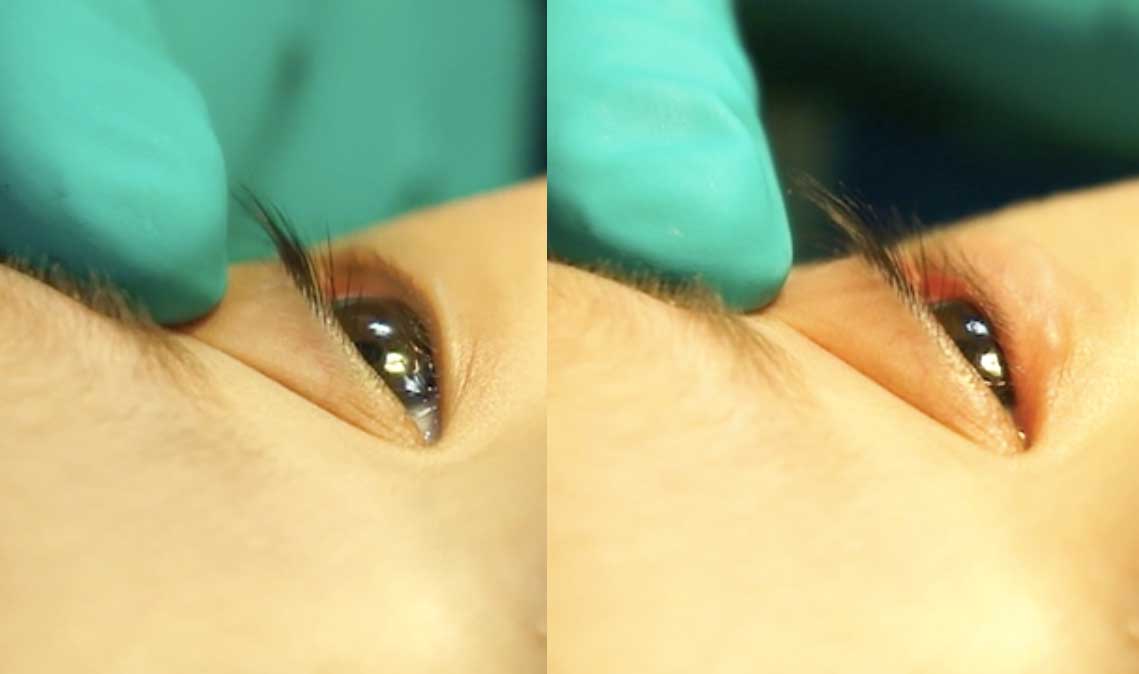
Figure 2: On the left side note the eyelashed rubbing the cornea. The right side image is immediately after the filler injection and the lashes are off the cornea with outward turning of the eyelid.
There are several advantages of treating epiblepharon with a filler injection. It is a minimally invasive nonsurgical option and is completely reversible. It allows temporary out- turning of lashes, allowing observation while spontaneous resolution is awaited. It avoids surgical excision and the attendant risk of overcorrection and ectropion.
2. Lagophthalmos:
Facial nerve palsy is a common cause for epiphora and redness of the eyes among patients. Facial nerve is the motor nerve to the orbicularis oculi muscle. The orbicularis oculi muscle is responsible for maintaining the tone of the lower lid along with the medial and lateral canthal tendons and the tarsus. The orbicularis oculi contractions that occur during blinking are responsible for the ‘lacrimal pump’, which drains tears from the tear lake over the punctum. Therefore, facial nerve palsy, which leads to paralysis of the orbicularis, causes reduction in the force of eyelid closure. This disrupts the lacrimal pump as well as the spread of the tear film across the corneal surface, which is required for wellbeing of the ocular surface. As a result, patients with facial palsy may often present with epiphpora, lagophthalmos, exposure keratopathy and congestion of the conjunctival surface.
Facial nerve palsy in many cases, may show spontaneous partial or complete recovery. However the issues experienced by the patient duration of the palsy can be very distressing for the patient. Treatment can be conservative with lubricants and measures such as eyelid taping being advised in mild cases of lagophthalmos. In moderate or severe cases other surgical measures such as palpebral springs, tarsorrhaphy or a gold weight may be used to treat the lagophthalmos. However, eyelid gold weights have the associated complications of fibrosis, extrusion, exposure, infection and granuloma formation in addition to being expensive.
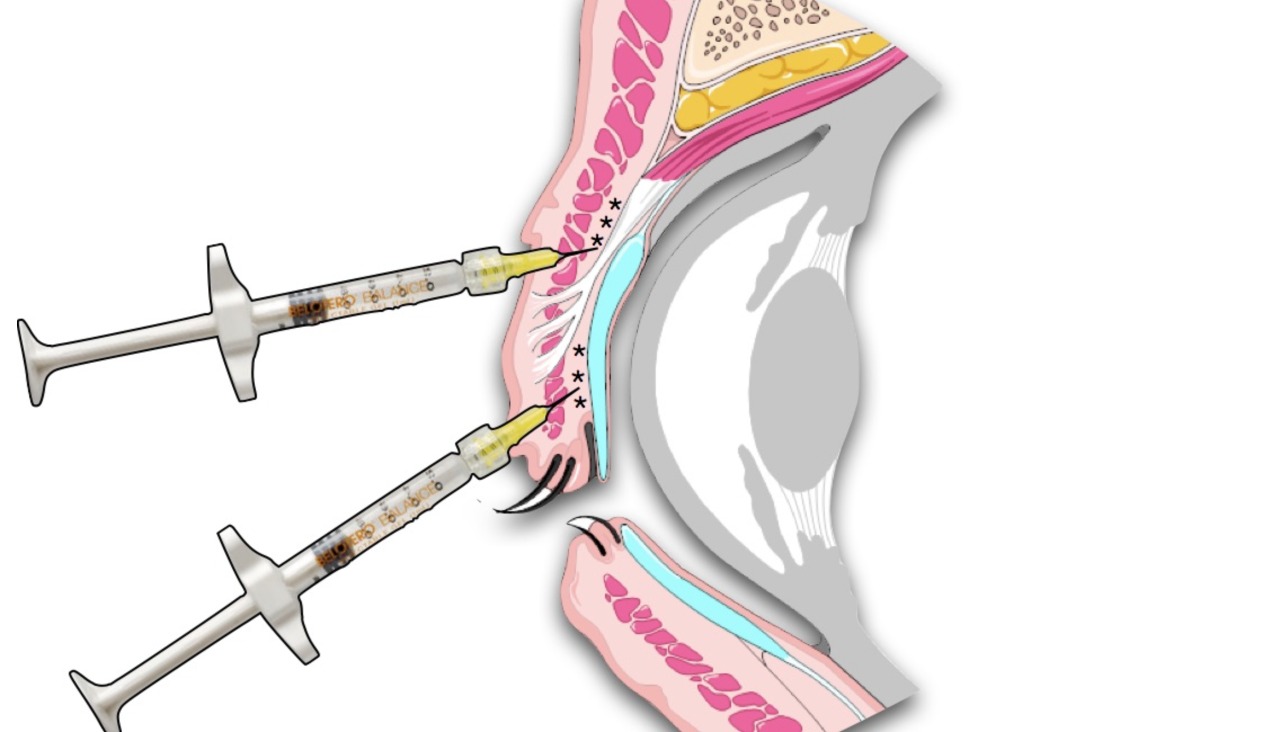
In cases where recovery of facial nerve function is expected, it may be prudent not to perform a permanent procedure like gold weight implantation or a tarsorrhaphy, which requires a second surgery to reverse it. Here, a hyaluronic acid filler may be used a a physiological ‘gold weight’. The filler can be injected in the upper eyelid area in the pretarsal and preseptal planes to add volume and weight to the upper eyelid therefore mechanically bringing the eyelid down during closure and reducing the lagophthalmos.
Figure 3: The exact plane for injecting the hyaluronic acid gel in the upper lid. The black asterisks demonstrate the filler material.
As Mancini et al. have demonstrated, hyaluronic acid fel for the correction of paralytic lagophthalmos offers many advantages: it is ideal for poor surgical candidates or mentally unstable patients. The temporary effect of the filler offers the capability to adjust the eyelid position in those patients in whom the underlying problem may be constantly changing. Also being minimally invasive, it avoids all the potential complications that are associated with a surgery; namely infection, hematoma and anesthesia related issues.
Figure 5: A 34 year old male with a history of recent onset facial palsy presented with epiphora and lagophthalmos (above). He underwent upper lid filler injection with Juvederm and post injection, observe the reduction in palpebral fissure height and the improvement in lagophthalmos.

Therefore, with appropriate case selection, patients of conditions such as epiblepheron and paralytic lagophthalmos can benefit from minimally invasive procedures like fillers to give effective and satisfactory outcomes.
References:
- Taban M, Mancini R, Nakra T, et al. Nonsurgical management of congenital eyelid malpositions using hyaluronic Acid gel. Ophthal Plast Reconstr Surg. 2009;25:259–63.
- Naik MN, Ali, MJ, Das S, Honavar S. Nonsurgical Management of Epiblepharon Using Hyaluronic Acid Gel. Ophthal Plast Reconstr Surg. 2010;26;215-17.
- Mancini R, Taban M, Lowringer A, et al. Use of Hyaluronic Acid Gel in the Manageent og Paralytic Lagophthalmos: The Hyaluronic Acid Gel “Gold Weight”. Ophthal Plast Reconstr Surg; 2009;25;23-26
By,
Akshay Gopinathan Nair, DNB,
Ophthalmic Plastic Surgery & Ocular Oncology,
Advanced Eye Hospital & Institute,Navi Mumbai
Aditya Jyot Eye Hospital, Mumbai
www.drakshaynair.com
